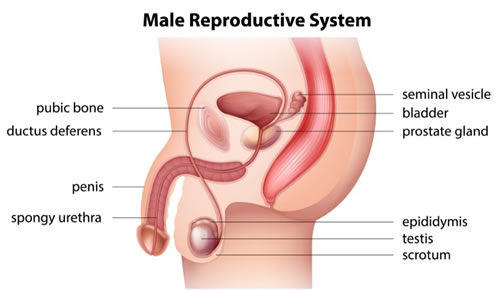
The testicles are two small oval shaped organs which hang below the penis in a pouch of skin called the scrotum. They are part of the male reproductive system. From the age of puberty the testicles produce sperm which can fertilise the female egg.
The collecting tubules inside the testicle join together to form a tube called the epididymis. This tube carries on and gets wider as it leaves the testicle. This wider tube is called the spermatic cord. The spermatic cord continues to form a short tube called the ejaculatory duct. This duct opens into the urethra (the tube from the bladder to the end of the penis) just above the prostate gland.
During ejaculation, sperm move from the epididymis, up the spermatic cord to the ejaculatory duct. They are mixed with liquid called semen and forced out of the penis. The testicles also produce the hormone testosterone.
What is male factor infertility?
When the sperm count is Iow, absent or the sperm are abnormal the chances of normal conception are reduced. A male factor problem can usually be identified in 50% of cases. If you have been having regular, unprotected intercourse for 12 months or longer without achieving a pregnancy, a simple semen analysis (sperm test) can be arranged to evaluate the quality of the sperm.
Low sperm counts
Historically, male sperm counts have been dropping globally over the last 30 years but no obvious cause has been identified. A number of medical conditions or lifestyle factors may contribute to a low sperm count. We can advise on appropriate testing to exclude any common causes (e.g. varicocele) and identify possible reversible factors that may respond to treatment.
Azoospermia
The absence of sperm in the ejaculate is termed azoospermia and is determined by looking at your semen sample down a microscope. If there are no sperm present it can be due to a blockage between the testis and the urethra (obstructive) or due to poor sperm production or spermatogenesis (non-obstructive)
- Obstructive (OA): blockages may appear as a result of a congenital problem, infection, inflammation or previous surgery. Sperm production is usually normal and it may be possible to reconstruct the problem microsurgically to allow normal conception.
- Non-obstructive (NOA): usually low or failure of spermatogenesis reflects a problem within the testis or the pituitary gland. The normal mechanism for sperm production may have been affected by external toxins, trauma, infection, cancer or hormone imbalance.
Vasectomy
Vasectomies are usual performed in men who have completed their family and want to be permanently sterilised. The procedure can be performed under local or general anaesthesia and takes approximately 20 minutes. We will fully counsel you about the potential risks of surgery and what to expect during your recovery. These operations are routinely performed by urological surgeons with a high degree of success. LEEDS UROLOGY PARTNERSHIP can usually provide counselling and treatment within 7 days at any of our clinics at a time to suit you.
Vasectomy reversal
Mr Oliver Kayes (Consultant Uro-Andrologist) performs vasectomy reversal routinely as part of his clinical practice. He trained in microsurgical techniques in London and offers a comprehensive portfolio of treatments to maximise your chance of having a baby. In his role as the Uro-Andrologist at the Leeds Centre for Reproductive Medicine (LCRM) he can offer simultaneous sperm retrieval and freezing for anyone undergoing vasectomy reversal. This approach keeps all options open for the couple going forward and avoids a second surgery at a later date. Mr Kayes will carefully counsel you about your chances of success (patency & pregnancy rates) based on your individual case (time since vasectomy, female age and fertility, clinical assessment). Fundamentally, success rates drop as the time since vasectomy extends beyond 10 years. Mr Kayes is happy to report a number of successful cases beyond this time point and also for men undergoing a second procedure in whom the initial vasectomy reversal had not worked.
Microsurgical technique
It is important to establish a consultation to discuss all the options available and for you to meet Mr Kayes in person before deciding on a surgical treatment. He will review the information pertinent to your fertility and any previous surgery. A clinical examination is required in order to decide on the chances of success and the optimum surgical approach. A methodical approach allows best planning, short procedure times and fast recovery. The vas deferens is reconstructed using a single layer anastomosis with de-tensioning sutures. After surgery, the scrotum may swell and bruise and be a little uncomfortable. You are required to rest and avoid any sexual activity for 2 weeks and finally perform a semen analysis at 3 months.
Tests & treatments
- Full clinical assessment
- Gene testing
- Sperm testing and storage
- Sperm optimisation and nutritional support
- Surgical sperm retrieval: percutaneous or microsurgical
- Microsurgical varicocele ligation
- Electroejaculation
