Men are notoriously poor at seeking help or assessment for their own health problems. One in five men has not seen a doctor in the past three years. Two-thirds of men have a family history of cancer, stroke and heart disease but more than half have not had basic healthcare checks in the last year.
Key men’s health statistics:
- 40% of men still die prematurely (before the age of 75).
- 1 in 5 men die before the age of 65.
- Coronary heart disease kills more men than women and on average men develop it 10-15 years earlier.
- Men are 60% more likely than women to develop a non sex-specific cancer, and are 70% more likely to die from the disease.
- Men are more likely to drink alcohol above recommended levels, smoke cigarettes and eat a poor diet
- By 2015, 36% of men will be obese and, by 2025, only 13% will have a healthy body mass index
- Three times as many men commit suicide
- Men visit their GP 20% less frequently than women
Key male urology facts:
- 50% of men between the ages of 40 to 70 suffer from some degree of erectile dysfunction
- Peyronie’s disease may affect as many as 1 in a 1000 men in UK
- 1 in every 10 men are worried about penile size
- Prostate cancer is the most common form of male cancer
- Globally sperm counts are declining
- Diabetes amongst men is increasing and is linked to sexual problems, bladder issues and higher rates of UTI
- Low testosterone affects 40% of men over age 45 years and may be linked to earlier death
LEEDS UROLOGY PARTNERSHIP aims to provide a holistic approach to male health issues and provide expert care for men suffering from urological illnesses.
Sexual dysfunction
Whilst the stigma and barriers around men talking about their personal problems with sexual dysfunction have improved over the last two decades; without doubt it remains a sensitive and embarrassing topic for most men. LEEDS UROLOGY PARTNERSHIP are at the forefront of these innovations and provide a private & friendly environment to discuss any personal matters.
Often men feel isolated and under pressure to match up to the typical male stereotypes portrayed in the press and media. We can help you understand your problem and put it into a broader context with our unique experience treating patients with different problems in our clinics. Typically, men will seek help with the one or more of the following problems:
- low libido, poor orgasm
- ejaculatory dysfunction: premature, delayed or failure/retrograde
- erectile dysfunction
- penile curvature
- painful intercourse
- associated urinary symptoms
We often see an overlap of these conditions affecting men without prior warning causing significant distress and poor quality of life. Similarly, men suffering the side-effects of previous chronic illness or surgical treatments (e.g. radical prostatectomy) rely on us to restore both their confidence and sexual relationships.
We provide detailed and personalised care to every man in order to understand the underlying issues and identify focal treatments with proven benefit. Our experience allows us to access the latest technology for testing and treating men to achieve the best clinical outcomes.
LEEDS UROLOGY PARTNERSHIP offers the following services:
Diagnostic
- Hormone profiling
- Cardiovascular risk assessment
- Nocturnal Penile Tumescence (NPT)/Rigiscan testing
- Penile duplex ultrasound
- Penile curvature assessment & treatment planning
Treatments
- Lifestyle advice and rehabilitation programmes
- Psychosexual counselling & psychotherapy
- Medical therapies: PDE5 inhibitors (e.g. Viagra), prostaglandin creams (e.g. Vitaros) & prostaglandin injections (Caverject; Invicorp)
- Testosterone replacement therapy
- Non-invasive therapies: acupuncture
- Mechanical therapies (vacuum device, traction device, vibrostimulation)
- XiapexTM injection and modelling for Peyronie’s disease
- External Shockwave Therapy (ESWT) for erectile dysfunction and Peyronie’s disease
- Surgical (corporoplasty (e.g. Nesbit), penile lengthening (e.g. grafting), penile implants)
Penile cancer
Penile cancer is a rare malignancy with approximately 1000 men affected each year in the UK. Leeds is one of 12 UK specialist centres selected to deliver care to these men and Mr Oliver Kayes holds unprecedented clinical and research experience in treating this rare condition.
The goals of treatments are:
- Accurate diagnosis and staging
- Oncological cure
- Preserve penile length and function using innovative reconstructive techniques
- Utilise sentinel node biopsy
- Safe and accurate surveillance
- Referral for adjuvant chemotherapy, radiotherapy or targeted treatments
Associated dermatological conditions such as balanitis xerotica obliterans (BXO) and generalised genital health will be expertly assessed and treated.
Access to collaborative clinical trials and contemporary research updates. More information available at the LTHT and Orchid website.
Penile surgery and other treatments
The following procedures are routinely performed by Mr Kayes (Uro-Andrologist) and his team:
- Circumcision
- Frenuloplasty
- Skin grafting
- Penile lengthening
- Testicular implants
- Liposuction/Fat excision
Testicular cancer
Approximately 2,300 new cases of testicular cancer in the UK in 2012
Testicular cancer has an unusual relationship with age: it is more common in younger men than in older men, with more than 8 in 10 cases diagnosed in the under 50s.
Most testicular cancers occur in descended testicles.
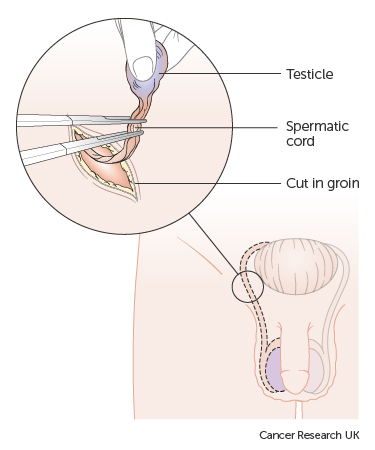
Most men have the whole testicle removed in order to diagnose the cancer. This operation is called an orchidectomy.
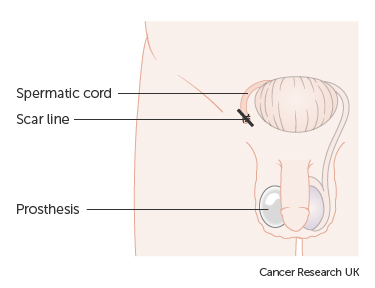
We can replace the testicle with a false one, called a prosthesis or a testicular implant. This will mean that your scrotum appears normal after your operation. In some men with very small tumours the surgeon removes only part of the testicle (partial orchidectomy)
The diagrams below show how the surgeon removes the testicle and the position of the scar line and prosthesis after surgery.
Your ability to have an erection and father a child will not be affected as long as only one testicle is removed and the remaining testicle is normal. Having cancer in both testicles is very rare. If you do have both testicles removed, you will no longer be able to father children. You will also need to take male hormone replacement treatment (testosterone).
Urethral stricture
The urethra (water-pipe) helps to pass urine outside the body. This thin tube also has an important role in ejaculation for men. When a scar from swelling, injury or infection blocks or slows the flow of urine in this tube, it is called a urethral stricture.
In males, the urethra is divided into posterior and anterior urethra.
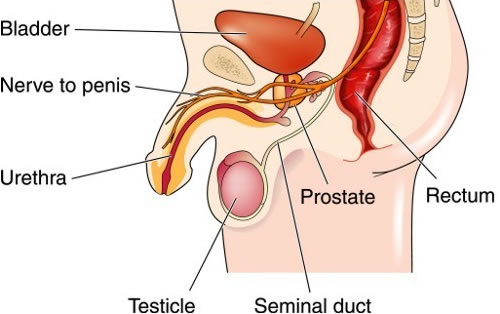
The posterior urethra includes:
- the bladder neck (the opening of the bladder)
- the prostatic urethra (the part of the urethra by the prostate)
- the membranous urethra
- a muscle called the external urinary sphincter
The anterior urethra includes:
- the bulbar urethra (under the scrotum and perineum- the area between the scrotum and anus)
- the penile urethra (along the bottom of the penis)
- the meatus (the exit at the tip of the penis)
Urethral strictures can be treated in a variety of ways including:
Urethral dilatation
Using specially designed dilators we can restore the normal calibre of the urethral lumen under local or general anaesthetic. As the scar is not removed, repeated treatments of self-dilatation with a catheter is often required.
Urethrotomy (“cutting the scar”)
For simple strictures it is usually possible to pass a telescope down the urethra and simply cut the scar which will release to a normal diameter. A catheter is usually inserted temporarily to prevent any bleeding. Strictures can recur in approximately 50% of cases.
Urethroplasty (surgical reconstruction)
- Hypospadias
- Penile
- Bulbar
For recurrent or complex strictures, a more definitive procedure is often required that will substitute healthy tissue once the scar has been excised. The graft may be taken from inside the mouth and a catheter left for 2 weeks to allow complete healing of the new urethra. Depending on the nature and location of the stricture it may be necessary to complete the surgery over 2 stages (i.e. 2 operations) to ensure the best outcomes. Depending on the specific surgery complications include: recurrent stricture, failure for graft to take, ejaculation or erectile problems and post-micturition dribbling. Urine flow is usually normal after surgery and long-term results are good.
Perineal urethrostomy (surgical diversion)
Occasionally depending on preceding surgery, the degree of scarring and availability of suitable graft tissue; you may be advised to have the water-pipe repositioned. In this case the external opening is moved to behind the scrotum (in the perineum) and voiding will occur in a sitting position.
