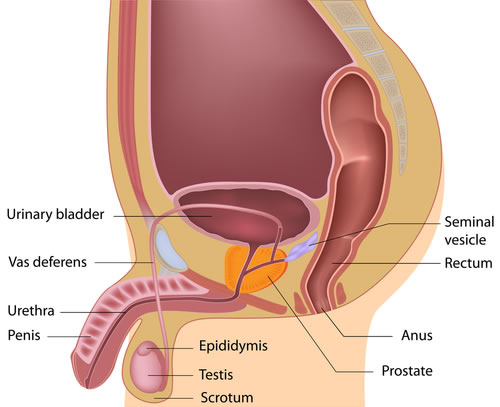
The prostate is part of the male genitourinary system. It is located beneath the bladder and in front of the rectum. Through the centre of the prostate passes the urethra, the tube that drains the bladder of urine. Only men have a prostate gland. It is usually the size of a walnut.
What does the prostate do?
The prostate gland is an important part of a man’s reproductive system. It helps produce semen, the fluid that passes from the penis during ejaculation alongside the seminal vesicles.
The prostate consists of 3 zones. The peripheral zone is located at the back of the prostate and is the part most susceptible to both prostate cancer and prostatitis. Enlargement of the prostate usually results from benign prostatic hyperplasia (BPH) developing in the transition zone, which lies in the middle of the gland and surrounds the urethra.
Symptoms to watch out for include:
- needing to urinate more often than usual, including at night – for example if you often need to go again two hours
- difficulty starting to urinate
- straining or taking a long time to finish urinating
- weak flow when you urinate
- a feeling that you’re not emptying your bladder fully
- needing to rush to the toilet – sometimes leaking before you get there
- dribbling urine after you finish.
Less common symptoms include:
- pain when urinating
- pain when ejaculating
- blood in your urine or semen
- problems getting or keeping an erection
Prostate Cancer
Facts
Prostate cancer is the most common cancer in men.
Over 44,000 men are diagnosed with prostate cancer every year – that’s more than 120 men every day.
Every hour one man dies from prostate cancer – that’s more than 10,500 men every year.
1 in 8 men will get prostate cancer in their lifetime.
Over 330,000 men are living with and after prostate cancer.
Embed: CaP statistics
Diagnosis – what is a PSA test?
Prostate specific antigen (PSA) is a protein that liquefies semen to aid fertility. It is continuously produced by the prostate in small quantities and is elevated in certain prostate conditions (e.g. cancer, inflammation and BPH). It can be measured in the bloodstream and helps guide diagnosis and response to treatment in some cases.
The test helps selects men who may be helped by further testing and a review by a urologist.
Transrectal Ultrasound (TRUS) and Multiparametric MRI (mMRI)
You may be offered a test to image your prostate in order to assess its shape, size and identify any abnormal areas. TRUS can be performed in the clinic and in some cases combined with prostate biopsy (see leaflet). mMRI can provide important information prior to prostate biopsy or surgery. MRI can also help diagnose causes for pelvic pain, infertility, congenital problems, assess pelvic floor defects associated with urinary incontinence.
Novel diagnostic biomarkers
The latest genomic and proteomic testing platforms are available to our patients to help guide difficult cases, provide family/hereditary testing or reassure men with abnormal results. We would be happy to discuss this service upon request.
Prostate biopsy – targeted or template or fusion technologies?
Our aim is to provide a full spectrum of diagnostic services to help diagnose and plan your treatments; whilst minimising the complications associated with repeated or random testing. Ultimately, we will map the location of any tumour to optimise biopsy protocols and provide maximal information to aid further treatment. Template biopsies are useful in men with prostate cancer on an active surveillance programme and men being assessed for suitability for focal therapy for prostate cancer. Prostate biopsies are taken through the perineum using a template to guide the position of the samples taken. This is done under general anaesthetic. The samples are then sent to a histology laboratory for examination under a microscope. The benefits of prostate mapping over TRUS and standard biopsy are a reduced rate of missing the cancer, a reduced rate of infection and bleeding also tends to be minimal. Prostate mapping is nearly always done in conjunction with MRI imaging.
Precision cancer testing – Oncofocus™
The world’s most comprehensive precision oncology test using novel gene sequencing techniques to identify the specific genetic mutations responsible for your cancer development and growth. These results are then matched to personalised, next generation cancer drugs to target your cancer.
Download a brochure
Treatments
LEEDS UROLOGY PARTNERSHIP helps men with prostate cancer through our:
- Dedicated psychological support and counselling
- Designing bespoke active surveillance protocols for individual cases
- Quick referral for radical treatment(s) including: Robotic prostatectomy, High Frequency Ultrasound (HIFU), Brachytherapy, Cryotherapy & Radiotherapy
- Optimisation of medical therapy
- Access to the latest international clinical trials
- Survivorship – join our group of men living beyond cancer with regular rehabilitation sessions, continence advice and restoring sexual relationships
Enlarged Prostate (BPH)
Male Lower Urinary Tract Symptoms (LUTS) are common in older men and often the result of benign prostatic enlargement. These symptoms can be bothersome and negatively impact on a man’s quality of life. Often the effects of getting up at night to void, passing urine too frequently or incontinence will lead to relationship problems.
BPH is a gradually progressive disease that often affects men aged 40 and above. Around 40% of men over 60 have lower urinary tract symptoms due to BPH, and quality of life is impaired in around half of these men.
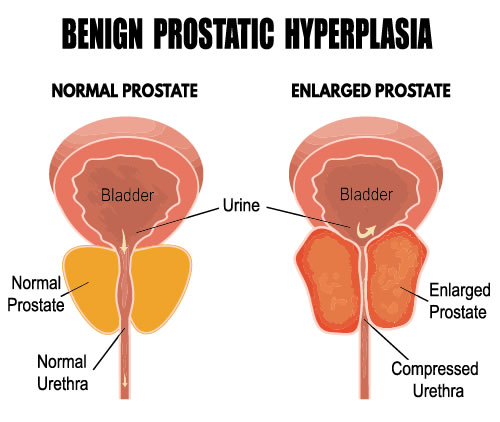
BPH refers to a non-cancerous growth of the prostate gland. This growth reduces the ability of the urethra to expand when passing urine, leading to problems urinating.
Bladder outflow obstruction due to BPH can cause the muscular bladder walls to thicken in certain men. This increases pressure within the bladder, which causes pouches (‘diverticula’) to form. This puts reverse pressure on the kidneys, leading to kidney problems over time. The bladder becomes unable to empty efficiently, triggering infections and bladder stones.
In some men male LUTS will overlap with other conditions including metabolic syndrome, sexual dysfunction and general health problems.
Diagnosis
- Bespoke assessment and tailored treatments
- Uroflowmetry (“pee in the bucket test” or “flow test”)
- Prostate volume measurement
- Risk assessment for urinary retention
Prior to any consultation we will begin to gather information about you and your problem using specially designed questionnaires and reporting systems. At our dedicated clinic you will first be asked to perform a flow test, so arrive with a comfortably full bladder. A digital rectal examination (DRE) and a transrectal ultrasound (TRUS) will help assess the prostate in detail. We can calculate the risk of your disease getting worse and help you pick the best treatment for you. You may be required to undergo a flexible cystoscopy in certain cases. PSA testing will be discussed.
Treatments
Dietary advice
The good news is that a diet rich in certain vitamins and minerals can keep your prostate healthy and lower your risk of BPH. We will also look at ways to help you lower both your weight and your overall risk of future problems.
Self-management strategies
Between 30-50% of men will be able to manage their own symptoms and a smaller proportion will actually see improvement overtime. We will design a bespoke programme with you that addresses your specific symptom complex and outline effective measures to see positive improvement. See health optimisation programmes
Medical treatments (alpha blockers, 5-alpha reductase inhibitors, PDE5 inhibitors)
Alpha blockers are drugs that relax the muscle at the bladder neck and improve urinary flow. They can cause postural hypotension (blood pressure drop on standing), retrograde ejaculation (reflux of semen into the bladder during orgasm) and dizziness. Please tell your doctor if you are due to have cataract surgery as this can be affected by this medication.
5 alpha reductase inhibitors (e.g. finasteride, dutasteride) block the conversion of testosterone, which encourages prostate growth, into its more active and potent form. This results in prostate shrinkage (about a third over 3-6 months), a fall in your PSA (about 50%) and symptom improvement. They can cause a reduction in libido, erectile dysfunction and breast enlargement/tenderness.
Combination therapy of the above has been shown to be more effective than either drug alone in men with enlarged prostates. These drugs may also be used in conjunction with antimuscarinic agents which help to stop bladder spasms.
PDE5 inhibitors: drugs commonly used for erectile dysfunction can reduce symptoms, especially in men with both erectile dysfunction and an enlarged prostate.
Plant extracts: a variety of these are available e.g. Serenoa repens and Pygeum africanum, the evidence for their use is weak but side effects are usually limited.
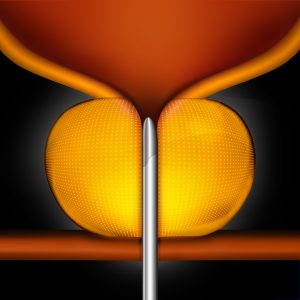
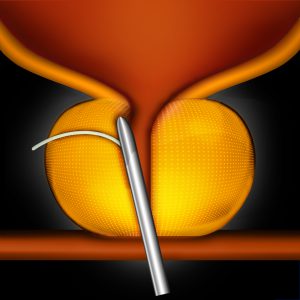
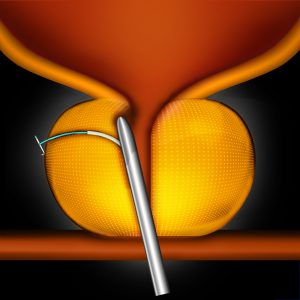
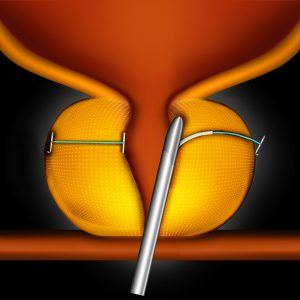
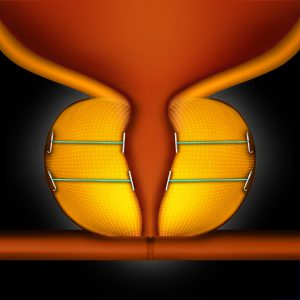
Urolift (Prostatic Urethral Lift)
This is a new procedure that involves pulling the sides of the prostate apart like a pair of curtains. The position is held using specially designed surgical staples. The major benefits include:
- minimally invasive day surgery with no cutting
- treatment under local anaesthesia (if desirable)
- minimal bleeding & no need for catheters after surgery*
- preserve sexual function
‘Urolift – Stuart’s Story’
This video follows Stuart through his initial consultation and assessment with Mr Oliver Kayes. Watch how he decides which men with BPH would benefit from Urolift surgery and the journey to symptom improvement for Stuart.
Urolift appears to perform best for men who have moderately enlarged prostates (30-80cc), fail medical treatments or have suffered significant side effects from medication.
We have successfully treated men with prostate size greater than 100cc and with middle lobe enlargement.
Mr Kayes is Chief Investigator for the PULSAR study assessing the impact of Urolift in men with urinary retention.
Bipolar TURP
The traditional surgical treatment for enlarged prostates involves passing a camera and special instrument up the urethra to allow removal of prostate tissue. This generates a wider channel faster and easier voiding. Sexual dysfunction including ejaculatory and erectile problems is common. However, complications such as incontinence or the need for a blood transfusion are rare.
Laser prostatectomy – Holmium Laser Enucleation of Prostate (HoLEP)
LEEDS UROLOGY PARTNERSHIP offers HoLEP surgery for all sizes or prostates. Unlike other laser operations on the prostate we strongly feel that HoLEP provides the best way to remove prostate tissue whilst minimising risks and speeding up recovery for patients. The goal is to remove as much tissue as possible to allow normal voiding and prevent re-growth and recurrent symptoms. There is often less bleeding so it is safe to use in men on anticoagulant medication (e.g. warfarin) and often catheters can be removed earlier. It is more suitable than TURP for very large prostates (>100cc). Long-term results appear very robust.
You can compare the treatments in the chart below:
[Table – Urolift versus other treatments- to follow]
Prostatitis and Complex Pelvic Pain Syndrome (CPPS)
Prostatitis can be acute or chronic (with or without infection) and often affects a man’s quality of life and may lead to anxiety and depression. Seeking medical attention and treating symptoms early can help to prevent long lasting issues.
Symptoms of prostatitis:
- Pain in the perineum/prostate (area between the anus and scrotum)
- Pain in the penis and/or testicles
- Pain in the lower back, rectum or inner thighs
- Chills and fever
- Frequency and/or urgency of voiding
- Incomplete bladder emptying
- Pain during or after ejaculation
- Blood in the semen (haematospermia)
Chronic pelvic pain is easily and often misunderstood. However, for those men and women who live with constant or severe pain, CPPS can seriously affect their daily lives. As with chronic pain elsewhere in the body, particularly loin and genital pain, it can be difficult to find a direct cause. We will ensure that using combination of a careful clinical examination and suitable tests (e.g. MRI) that we diagnose and treat any reversible causes for your pain. We also adopt a number of internationally recognised therapies targeting symptom relief, addressing associated physical or psychological problems and supporting you throughout your care.
Prostatitis & CPPS Treatment
LEEDS UROLOGY PARTNERSHIP works with multidisciplinary teams to provide dedicated and specialist treatment for your symptoms:
- Detailed investigations to rule out any causes or infective organisms
- Genomic testing for resistance, susceptibility traits, bacteria-isolation and targeted treatments
Drugs:
- Alpha blockers to relax prostatic ducts
- Antibiotics if any infection is suspected
- NSAIDs; non-steroidal drugs such as ibuprofen
- Opioid painkillers to control pain
- Muscle relaxants such as diazepam and baclofen
- Neuropathic agents: Amitriptyline, pregabalin and gabapentin
Surgery:
- Prostate massage
- Microsurgical denervation
- Nerve blocks
- Botox injection
- Referral for assessment and treatment by spinal cord stimulation
- Referral for assessment and treatment by robotic prostatectomy
Ejaculation disorders
see haematospermia, painful ejaculation, premature ejaculation, retrograde ejaculation, delayed/failed ejaculation.

